Management of ovarian endometrioma
What is an endometrioma?
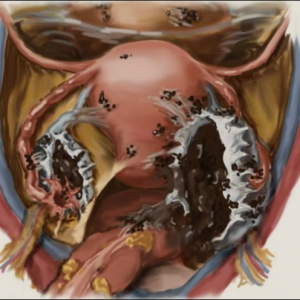
Endometriosis is a condition in which endometrium-like tissue grows in locations outside the uterus. When endometriosis occurs in the ovary, endometriotic cells can form a menstrual fluid-filled sac. This is called endometrioma, endometriotic or ‘chocolate‘ cyst due to the appearance of old-blood pigmentation.
How common is endometrioma found?
The exact prevalence of endometrioma is unclear, but may be detected on ultrasound in 15-40% of women with symptoms (pain or infertility) suggestive of endometriosis.
The presence of endometrioma is often a marker for co-existing deep endometriosis elsewhere in the pelvis, including the bowels and urinary tract
What is the ‘best‘ treatment for endometrioma?
There is no uniform agreement on the single ‘best‘ treatment for endometrioma. While surgical removal is the traditional treatment approach, the best management should be based on individual patient’s factors including type and severity of symptoms, age, fertility and treatment goals (reducing pain, maintaining fertility,excluding malignancy).
The choice of treatment options therefore varies from person to person and from time to time. Fundamentally, the management options include:
- expectant management
- medical therapy
- surgical therapy
Expectant management
This is an option when endometrioma is small, has ultrasound appearance consistent with a benign cyst and causes no symptoms.
Medical management
A variety of medical therapies are available to alleviate pain associated with endometriosis / endometrioma. These include Nonsteroidal anti-inflammatory drugs (NSAIDs), oral contraceptives (OCs), Progestins (Medroxyprogesterone acetate, Dienogest), GnRH analogs).
In general, drug treatment of ovarian endometrioma is not curative because drug does not eliminate cyst formation. This means that the endometrioma may enlarge or become symptomatic once medical treatment is ceased.
Surgical management
There is no consensus or high-quality evidence to guide decision-making in every situation. However, surgical removal of endometrioma may be appropriate when:
- endometrioma is large (≥4 cm arbitrary cut-off)
- pain related to endometriosis / endometrioma is severe
- when malignancy cannot be excluded
There is consensus behind the use of laparoscopic surgery rather than open laparotomy for treatment of endometrioma as the former is associated with shorter hospital stay, faster recovery, less analgesic requirements, decreased costs, and lower incidence of adhesions.
Should infertile women undergo surgical removal of ovarian endometrioma?
The answer to this important question is contentious due to the lack of high-quality evidence and conflicting expert opinions. While the precise cause of endometriosis-related infertility remain uncertain in individual cases, the proposed mechanisms include (i) chronic inflammation, (ii) tuboperitoneal anatomic distortion, (iii) compromised ovarian reserve Iv) poor oocyte or embryo quality and (v) reduced endometrial receptivity.
It is generally accepted that (i) fecundity rates may be reduced in women with endometriosis (ii) women with endometrioma undergoing IVF have lower oocyte yield per cycle, higher cancellation rate and (iii) the presence of ovarian endometriomas is usually associated with moderate or severe disease elsewhere in the pelvis.These reasons would appear to support surgical treatment of endometrioma.
However, it is also recognised that:
- surgical intervention for endometrioma may reduce the ovarian reserve (reflected by decreased serum AMH levels)
- surgical treatment of endometrioma has not been shown to alter the outcome of IVF compared to those with untreated endometrioma
- women with endometrioma going through IVF have similar live birth rates (LBR) compared to women with no endometriosis
This conflicting evidence is because there are no randomized trials comparing laparoscopic excision to expectant management before IVF–ICSI cycles.
Surgery for severe endometriosis, including endometrioma, may be considered before IVF in the following cases:
- when the pain related to endometriosis is severe
- when malignancy cannot be excluded
- In patients with endometrioma ≥3 cm, laparoscopic ovarian cystectomy is recommended before IVF to reduce the risk of infection during oocyte retrieval and facilitate access to follicles, or to improve the ovarian response to controlled ovarian stimulation (2014 European Society of Human Reproduction and Embryology guidelines)
- when the qualities of the oocytes and embryos were found to be poor in IVF cycles before surgery, or in cases of recurrent implantation failure
Hence, individualisation of care for women with pelvic endometriosis and endometrioma-associated pain and subfertility is important to optimise outcomes.
https://www.sydneycare.com.au/wp-content/uploads/2021/01/Management-of-ovarian-cyst
